For over three months, the NBC 6 investigators have been surveying health care workers across South Florida getting their reaction to the coronavirus crisis in real time. Over 300 frontliners have participated since March.
The most recent results show they are worried.
More than eight of 10 of those who responded say they are “extremely” or “very” concerned about the number of infections.
They attribute the new wave of coronavirus cases to many reasons, including: “lack of social distancing,” “not wearing a mask,” “bad leadership,” ”reopening too early” and recent protests against police brutality.
“Unfortunately, we are back to square one, I believe,” said emergency physician Jorge Infante.
Infante says the percentage of patients testing positive for the virus at his facility is higher than ever before.

“If you are seeing greater numbers of people getting infected, just by sheer math, you are going to start seeing more complications so we are seeing sicker patients,” Infate said.
Local
As concerns grow among frontliners, more are questioning the actions of authorities.
In May, 64% of participants said local and state authorities were doing enough to keep residents safe.That number is down to 39% in the most recent survey.
Some, including Infante, are asking leaders for more testing, contact tracing and a clear message, which they say haven’t seen lately.
“I don't know how much shutdown we gotta do but we have to go back to the strategy that we have to dampen this curve, '' said Martha Baker, the union chief for Jackson Health System workers.
More than three quarters of those surveyed believe parts of the reopening should be “rolled back” or “indefinitely delayed.”
Baker has been raising the alarm for days as the number of ICU beds available continue to shrink at Jackson hospital with nearly 90% occupied Thursday
“It’s tight - patients are being taken care of but it’s stressful on the staff right now and it's borderline dangerous if we continue to peak,” Baker said.
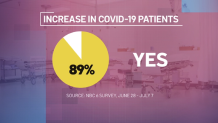
Nearly 90% of those who participated in this round of the survey say their workplace has seen an increase of infected patients. About half say they are enough resources to provide care. But 54% say they have “a great deal” or “a lot” of concern they will reach capacity.
“...I don’t know if it gets worse where the patients are going to go,” said Rublas Ruiz, an ICU nurse from Kendall Regional.
Ruiz says COVID-19 patients are quickly filling up the ICU units and there are not enough nurses to treat them.
“A lot of our workers in the hospital have been infected with the virus and not being able to go to work. That has affected our staffing,” Ruiz said.
He says the ratio for the intensive care unit is one nurse per two patients. But now, they are taking three patients each.

According to data released by the state, Kendall Regional’s ICU is 90% full.
In a statement, the hospital told us they “staff appropriately to the sickness level” of their patients and they have surge plans in place that include: using all available patient care space, restricting non-urgent elective procedures to preserve inpatient beds and the re-deployment of personnel and staff across all HCA’s healthcare system.
More than three quarters of those who participated in the survey have treated patients exposed to the virus and they say their symptoms are all over the place.
A nurse wrote: “Many people have varying symptoms from none, to mild stomach issues, to full on respiratory failure.” Another said: “At this time, symptoms are not as critical as before, though we have been treating a much younger generation.”

Ruiz says patients of all ages are now ending up in intensive care.
“Once you get it, it’s really difficult to get out of the effects of the virus. It’s not a common cold. It’s not a common flu,” he said.
Ruiz says patients with diabetes and hypertension are a higher risk of being intubated and not making it regardless of age.
“It’s been really sad,” Ruiz said. “We have done a lot to try to save these patients and sometimes you cannot do much for them.”



